Did you know that nearly half of adults over 50 experience hemorrhoids? These swollen veins in or around the rectum can cause discomfort, itching, and bleeding during bowel movements. But the good news? Most cases can be managed with simple lifestyle changes.
Key Takeaways:
- Common Causes: Low-fibre diets, dehydration, prolonged sitting, and straining during bowel movements.
- Prevention Tips:
- Eat fibre-rich foods like beans, kontomire, and fruits (e.g., mangoes, pears).
- Drink 2–2.5 litres of water daily.
- Avoid sitting for long periods and practice good toilet habits.
- Treatment Options:
- Home remedies: Sitz baths, aloe vera, and coconut oil.
- Medical care: Laser procedures or surgery for severe cases.
Hemorrhoids are common but manageable. Early action, like improving your diet and hydration, can prevent them from worsening. If symptoms persist, consult a doctor.
Doctor explains HEMORRHOIDS (aka piles) | Causes, symptoms, treatment & prevention
Basic Facts About Hemorrhoids
Hemorrhoids are clusters of blood vessels, smooth muscle, and connective tissue located in the anal canal. They play an important role in bowel control by contributing 15–20% of the resting anal pressure and providing sensory feedback. However, problems arise when these structures become swollen, inflamed, or prolapse. Around 11% of adults experience symptoms of hemorrhoids at any given time, and by the age of 50, nearly half of all adults have dealt with them. Let’s explore the different types and classifications of hemorrhoids.
Internal vs External Hemorrhoids
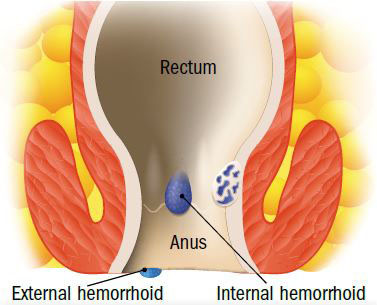
Hemorrhoids are categorized based on their location, which also determines their symptoms:
| Feature | Internal Hemorrhoids | External Hemorrhoids |
|---|---|---|
| Location | Inside the lower rectum | Around the anus |
| Visibility | Not visible without special instruments | Visible externally |
| Pain Level | Usually painless unless prolapsed | More likely to cause pain |
| Main Symptoms | Bright red bleeding during bowel movements | Swelling, itching, and discomfort |
| Nerve Endings | Fewer sensory nerves | A greater number of pain-sensing nerves |
Internal hemorrhoids typically form in three common areas within the anal canal: the left lateral, right posterior (the most frequent site), and right anterior regions. On the other hand, external hemorrhoids develop under the skin surrounding the anus. This distinction is essential for understanding the severity levels of internal hemorrhoids, which are discussed below.
4 Grades of Internal Hemorrhoids
Internal hemorrhoids are classified into four grades based on how severe they are:
- Grade 1
These are slightly enlarged but stay inside the anal canal. They may cause occasional bleeding but do not protrude outside the anus. - Grade 2
These prolapse during bowel movements but return to their normal position on their own. Bleeding may become more frequent. - Grade 3
Hemorrhoids that prolapse during bowel movements and need to be manually pushed back into place. This can cause significant discomfort. - Grade 4
These remain permanently prolapsed and cannot be manually repositioned. They often require immediate medical attention.
Straining during bowel movements can weaken the connective tissue that supports these vascular cushions, leading to their enlargement and displacement. Understanding these grades can help in identifying the appropriate treatment or management strategies.
Why Hemorrhoids Develop
Hemorrhoids often develop due to a mix of daily habits and genetic factors.
Diet and Daily Habits
What you eat and how you live play a big role in your risk of developing hemorrhoids. For instance, consuming less than 12 grams of fibre and drinking under 2 litres of water daily significantly increases the likelihood of hemorrhoids.
Here are some common dietary and lifestyle factors that may contribute to the problem:
| Factor | Impact on Hemorrhoid Risk |
|---|---|
| Low-fibre diet | Leads to straining during bowel movements |
| Insufficient water | Causes harder stools and constipation |
| Prolonged sitting | Increases pressure on anal blood vessels |
| Poor toilet habits | Results in unnecessary straining |
In Ghana, many local foods are great sources of fibre that can help reduce this risk:
| Food Item | Fibre Content |
|---|---|
| Navy beans (125ml) | 9.6 grams |
| Green peas (250ml) | 8.8 grams |
| Pear with skin | 5.5 grams |
“Internal hemorrhoidal disease was more frequently observed in patients with low-fiber diet and a reduced water intake. These dietary habits were described as precipitating factors of constipation which was found in almost all patients.”
When combined with other factors, poor dietary habits create the perfect conditions for hemorrhoids to develop.
Physical and Health Factors
Genetic Predisposition
Research has uncovered 102 genomic regions linked to hemorrhoid risk.
“Our findings indicate that hemorrhoidal disease results, at least in part, from dysfunction of smooth muscle, epithelial and connective tissue”.
Age-Related Factors
Age is another major contributor. Nearly half of people over 50 experience hemorrhoids. This is partly due to:
- Weakening of tissues that support the area
- Changes in bowel habits
- Decline in muscle tone
Other Contributing Factors
Additional conditions and activities that may raise your risk include:
- Pregnancy and childbirth
- Chronic constipation
- Heavy lifting
- Obesity
- Sedentary lifestyle
“Our PRS results need confirmation in other studies and various ethnic groups, but they could help identify people at higher risk of complications so they can be more closely monitored and benefit, to a greater extent, from healthy lifestyles to prevent surgical treatment”.
These factors, combined with diet and genetics, highlight the complex causes behind hemorrhoid development.
Signs and Symptoms
Spotting hemorrhoid symptoms early can help you avoid unnecessary complications.
Main Symptoms
Here are some common symptoms to look out for:
| Symptom | Description |
|---|---|
| Bleeding | Bright red blood during bowel movements |
| Discomfort | Itching, pain, or burning around the anus |
| Swelling | Tender lumps near the anal opening |
| Protrusion | Tissue bulging out during bowel movements |
Internal hemorrhoids often don’t cause pain right away because there are fewer nerve endings in that area. However, they can still bleed during bowel movements.
“Hemorrhoids are enlarged swollen veins in the anus and rectum.”
Research indicates that nearly 75% of adults will deal with hemorrhoids at some point in their lives. For pregnant women, the likelihood is even higher, with up to 35% experiencing hemorrhoids during pregnancy.
Although these symptoms are fairly common, certain warning signs mean it’s time to see a doctor.
Emergency Warning Signs
While some hemorrhoid symptoms can be managed at home, some require immediate medical attention. If you’re not sure or you’re worried you can book a consultation and speak to a doctor within 5mins on DrDoGood.
Severe Pain and Swelling
- Intense pain that keeps getting worse
- Large, painful lumps that can’t be pushed back in
- Blood clots forming inside the hemorrhoids
Bleeding Issues
- Heavy or ongoing rectal bleeding
- Dark red or black, tar-like stools
“You should never ignore rectal bleeding…your rectal bleeding may also be a sign of a more serious gastrointestinal condition such as colon cancer or inflammatory bowel disease.” – John Rivas, M.D., Gastroenterologist
If you experience additional symptoms like a fever over 38°C, chills, nausea, or a rapid heartbeat, it’s crucial to seek immediate care.
Persistent symptoms that don’t improve within a week of home treatment also warrant a visit to your doctor.
“That’s why it’s always better to be safe than sorry and get your hemorrhoids evaluated by a healthcare professional sooner rather than later.”
Other Concerning Symptoms
- Unexplained weight loss
- Ongoing abdominal pain
- Frequent diarrhoea or constipation
- Unexplained fatigue
Pay attention to these signs, as they could point to underlying issues that need professional evaluation. Early action can make all the difference.
How to Prevent Hemorrhoids
Taking steps to prevent hemorrhoids can make a big difference, especially when tailored to everyday habits and resources in Ghana.
Food Choices
Incorporating fibre-rich local foods into your meals is a simple way to keep things moving smoothly. Here’s a quick guide:
| Food Type | Local Examples | Fibre Content |
|---|---|---|
| Legumes | Black-eyed peas (cowpeas), bambara beans | 7–10 g per 1/2 cup |
| Vegetables | Kontomire, garden eggs, okro | 4–6 g per cup |
| Fruits | Mangoes, oranges, avocados | 4–5 g per serving |
| Whole Grains | Brown rice, millet, sorghum | 3–4 g per 1/2 cup |
“Fiber supplementation has been proven to reduce the incidence of bleeding and persisting symptoms in hemorrhoid patients by around 50%”
To hit the recommended daily fibre intake of 28 g, start small and increase gradually. This helps your digestive system adjust and reduces the risk of bloating.
Water and Toilet Habits
In Ghana’s warm climate, staying hydrated is a key part of keeping your digestive system running smoothly, especially when paired with a high-fibre diet.
Hydration Tips:
- Drink 2–2.5 litres of water daily.
- Kick-start your day with a glass of water.
- Cut back on dehydrating drinks like coffee and alcohol.
When it comes to bathroom habits, follow the ‘TONE’ strategy:
- T: Spend no more than three minutes on the toilet.
- O: Stick to a once-daily bowel movement routine.
- N: Avoid straining during bowel movements.
- E: Ensure your diet includes enough fibre.
“Drinking enough water might not be the first thing that comes to mind when thinking about hemorrhoids treatment, but staying well-hydrated plays a crucial role in both prevention and relief.” – Dr. Azhar Alam
Exercise Tips
Staying active is another way to prevent hemorrhoids. Regular movement improves circulation and supports digestion.
Good Activities to Try:
- Enjoy morning or evening walks in your neighbourhood.
- Swim at local pools or beaches.
- Practice simple yoga poses like Child’s Pose.
- Do pelvic floor exercises (Kegels), which you can easily perform while sitting or standing.
What to Avoid:
- Strenuous weightlifting or intense cycling.
- Overdoing squats or other high-strain exercises.
Treatment Methods
Hemorrhoid relief in Ghana can be achieved through a mix of home remedies and medical interventions.
Self-Care and Pharmacy Options
For mild to moderate hemorrhoid symptoms, home remedies and over-the-counter options can be effective.
Sitz Baths
Soaking in warm water for 10–15 minutes, two to three times daily, can help ease discomfort and reduce swelling. Adding Epsom salts, as recommended, may enhance the soothing effect.
Natural Remedies
Pharmacies stock natural options that can provide relief:
- Aloe vera gel: Helps soothe burning and itching sensations.
- Coconut oil: May calm irritation.
- Witch hazel: When applied, it can assist in shrinking swollen blood vessels.
“Hemorrhoids can be troublesome and embarrassing, but they often shrink on their own with simple self-help care and over-the-counter remedies.”
– Dr. Howard LeWine, Assistant Professor of Medicine at Harvard Medical School
Over-the-Counter Products
Local pharmacies offer a variety of solutions, including:
- Creams with hydrocortisone to reduce inflammation.
- Suppositories for internal hemorrhoids.
- Pain-relieving wipes for soothing discomfort.
- Anti-inflammatory medications to address swelling and pain.
Doctor-Provided Treatments
If home remedies don’t provide relief, medical treatments can address more severe cases.
Minimally Invasive Procedures
Laser Hemorrhoidoplasty (LHP) is a modern, minimally invasive option available in major medical centres across Ghana. This procedure uses laser energy to treat hemorrhoidal tissue effectively, offering several benefits:
- Operative time is relatively short, averaging about 29.67 minutes.
- Patients experience less pain after the procedure.
- Most individuals can return home the same day.
- There’s a lower chance of complications like anal stenosis or incontinence.
For added convenience, platforms like DrDoGood provide virtual consultations starting at 45 GHS. This service allows you to discuss symptoms and explore treatment options from the comfort of your home, complementing self-care methods with professional guidance.
Surgery Options
When self-care and less invasive treatments aren’t enough, surgery often becomes the go-to solution. For Grade III or IV hemorrhoids, surgical intervention is usually necessary when non-surgical methods fail.
Current Surgical Methods
Surgery is required in less than 10% of hemorrhoid cases.
Traditional Hemorrhoidectomy
This is one of the most effective surgical methods, boasting success rates as high as 95%. It comes in two variations:
- Closed Hemorrhoidectomy: The hemorrhoidal tissue is removed, and the wound is stitched up using absorbable sutures.
- Open Hemorrhoidectomy: Similar to the closed method, but the surgical site is left open. This approach is often chosen when there’s a higher risk of post-surgery infection.
Advanced Techniques
These newer methods aim to reduce pain and speed up recovery:
- Stapled Hemorrhoidopexy (PPH): A circular stapler is used to remove excess tissue, significantly reducing post-surgery discomfort.
- Doppler-guided Hemorrhoidal Artery Ligation: Ultrasound technology helps locate and tie off hemorrhoidal arteries, making it a good option for Grade II–III cases.
- Transanal Hemorrhoidal Dearterialization (THD): This technique reduces blood flow to the hemorrhoids and is effective for specific patients.
The type of surgery chosen plays a major role in shaping the recovery process, which is outlined below.
Recovery and Aftercare
Post-surgery care is all about ensuring a smooth recovery, which typically takes 2–8 weeks. Key steps include:
- Taking sitz baths for comfort and hygiene
- Using prescribed pain medications
- Increasing fibre and water intake to prevent constipation
- Gradually returning to daily activities
Important Considerations
Certain factors make surgery the right choice, including:
- Non-surgical treatments haven’t worked
- Hemorrhoids are severely prolapsed
- Complications like strangulation arise
- Both internal and external hemorrhoids are present
- Coexisting anorectal conditions need attention
The decision on which surgical method to use depends on the hemorrhoid’s location and severity, your overall health, how you’ve responded to past treatments, and personal preferences.
While surgery might seem intimidating, it often leads to significant, long-lasting relief. Many patients report a noticeable improvement in their quality of life after undergoing surgical treatment.
Long-Term Care and Prevention
Sustaining lifestyle changes after treatment plays a vital role in maintaining long-term wellness. Research indicates that adopting healthier habits can significantly reduce the risk and severity of hemorrhoids.
After-Treatment Care Steps
“Everyone has hemorrhoids… It’s only when these blood vessels start to swell and become inflamed that they present a problem that can be quite painful.”
Prioritising Hygiene
- Use water or gentle wipes to clean the area after bowel movements.
- Take 15–20 minute sitz baths two to three times daily.
- Ensure the area is thoroughly dried afterward.
Dietary Adjustments
- Aim for a daily intake of 28 grams of fibre, paired with 2 litres of water.
Adding high-fibre foods to your diet can help with sustained recovery. Here are some excellent options:
| High-Fibre Food | Portion Size | Fibre Content |
|---|---|---|
| Navy beans | 1/2 cup cooked | 9.6 grams |
| Raspberries | 1 cup | 8.0 grams |
| Green peas | 1 cup cooked | 8.8 grams |
| High-fibre bran | 1/2 cup | 14.0 grams |
Daily Habit Changes
“To prevent hemorrhoids, you want stool that is soft and easy to pass. You can reach the right consistency by making smart diet choices and drinking plenty of water to avoid dehydration.”
Here are some practical adjustments to support prevention:
- Act promptly when you feel the urge to use the toilet.
- Limit time spent on the toilet to no more than 2 minutes.
- Take regular breaks from prolonged sitting.
- Incorporate regular exercise and avoid heavy lifting.
- Work towards maintaining a healthy weight.
Dietary Tips
- Include flavonoid-rich foods like berries and citrus fruits in your meals.
- Cut back on spicy foods if they tend to trigger symptoms.
- Reduce alcohol and caffeine consumption.
These small yet impactful changes can complement immediate care efforts and help lay the groundwork for consistent management.
Using DrDoGood for Care
DrDoGood provides valuable tools and expert support for managing and preventing hemorrhoids:
Virtual Consultations
- Connect with specialists starting at just 45 GHS.
- Receive personalised advice on diet and overall wellness.
- Access ongoing monitoring and tailored care plans.
Condition Management
- Track symptoms to monitor progress.
- Get reminders for medications.
- Explore educational resources to stay informed.
Combining these steps with the expert support available through DrDoGood can help ensure a smooth recovery and promote lasting well-being.
Summary
Haemorrhoids are a common concern in Ghana, often interfering with daily routines. This guide has explored their causes, dietary prevention tips, proper hygiene practices, and treatment options to help you take control of managing them.
“The development and exacerbation of haemorrhoids can be closely related to one’s lifestyle and dietary habits. By making intentional choices in these areas, one can significantly reduce the risk and severity of haemorrhoids.” – King Edward VII’s Hospital
Addressing haemorrhoids effectively requires a proactive and informed approach.
Key Prevention Steps
Taking steps to prevent haemorrhoids involves focusing on three main areas:
| Focus Area | Key Actions | Benefits |
|---|---|---|
| Diet | Add more fibre to meals and drink at least 2L of water daily | Prevents constipation |
| Bathroom Habits | Avoid straining and limit time spent on the toilet | Reduces pressure on veins |
| Physical Activity | Exercise regularly and avoid heavy lifting | Encourages healthy blood flow |
These habits not only reduce the risk of haemorrhoids but also promote overall wellness. However, if symptoms persist, it’s important to seek professional advice.
When to Seek Professional Help
While prevention is the goal, some cases require medical attention. Consider consulting a healthcare provider, such as through DrDoGood’s virtual consultations (starting at 45 GHS), if you experience:
- Symptoms lasting more than a week
- No improvement with home remedies
- Bleeding during bowel movements
- Intense or worsening pain
Timely intervention can prevent complications and provide relief.
Long-term Management for Wellness
For ongoing relief and prevention, long-term lifestyle adjustments are crucial. Since haemorrhoids can recur, adopting sustainable habits is key. Here are a few strategies to consider:
- Include fibre-rich foods like whole grains, vegetables, and flavonoid-rich options such as berries and citrus fruits in your diet.
- Avoid sitting for extended periods; take regular breaks to move around.
- Use warm water for gentle anal hygiene to avoid irritation.
DrDoGood’s platform provides access to specialists who can guide you in managing haemorrhoids effectively. By combining lifestyle changes with expert care, you can achieve lasting comfort and improved quality of life.
FAQs
What are the early symptoms of piles, and when should I consult a doctor?
Early signs of piles (haemorrhoids) often show up as itching, pain or discomfort during bowel movements, swelling around the anus, or noticing bright red blood on toilet paper or in your stool. The severity of these symptoms can differ based on whether the haemorrhoids are internal or external.
It’s important to see a doctor if:
- Bleeding is heavy or doesn’t stop.
- Pain and swelling get worse or fail to improve with home treatments.
- Symptoms last longer than two weeks.
- You notice dark red blood in your stool, stools that are tar-like in texture, or experience unexplained abdominal pain or bloating.
Seeking medical advice early helps ensure an accurate diagnosis, proper treatment, and relief from discomfort.
What lifestyle changes can help prevent hemorrhoids from coming back?
To minimise the chances of hemorrhoids coming back, making some changes to your daily habits can make a big difference. Start with your diet: add more fibre-rich foods like fresh fruits, vegetables, and whole grains. Pair this with plenty of water to keep your stools soft and make bowel movements easier. Also, avoid straining when using the toilet and try to stick to a regular bathroom schedule.
Stay active – regular exercise not only boosts circulation but also helps prevent constipation. If you have a job that requires sitting for long hours, take short breaks to stretch or walk around. Keeping your weight in check is equally important since excess weight can put extra pressure on the veins in your rectal area.
These small but impactful changes can go a long way in reducing the risk of hemorrhoids returning while also supporting better digestive health overall.
What is the difference between minimally invasive treatments and traditional surgery for severe hemorrhoids?
Minimally invasive treatments, such as transanal hemorrhoidal dearterialization (THD), focus on cutting off the blood supply to the hemorrhoids. These procedures typically result in less pain and a shorter recovery time compared to more traditional surgical methods.
On the other hand, traditional surgeries like conventional hemorrhoidectomy involve completely removing the hemorrhoids. While this approach is highly effective for severe cases, it often comes with more post-operative pain and a longer recovery period.
Both options work well, but the best choice depends on the severity of the condition and your doctor’s advice.


Leave a Reply